Shedding the diabetes stigma: Say no to blame and shame
You're already checking your blood sugar, seeing doctors and educators and watching what you eat. Anyone who wants to judge you, including yourself, should be impressed by what you're getting right, not looking for ways to criticize. If you ever feel down on yourself for living with diabetes or worry that others might, try to do these four things for yourself: Believe you didn't cause diabetes. You've most likely been told or read that diabetes isn't your fault, but do you believe it? Whether you live with type 1...
Read MoreUnderstanding type 1 diabetes
What is it? Known as “insulin-dependent diabetes” or “juvenile diabetes", type 1 diabetes affects 5% to 10% of people living with diabetes. Type 1 diabetes requires immediate insulin treatment and occurs mostly in children and teenagers. What many people don’t know is that it can develop at any age and that it unfortunately cannot be prevented. Even today, the exact causes of the disease remain unknown. Genetics can play a role, and some environmental factors, such as viruses, can trigger the...
Read MoreUnderstanding Prediabetes
What is it? Prediabetes is when a person’s blood sugar level (blood glucose) is higher than average, but not enough to diagnose them with diabetes. Almost all people living with type 2 diabetes have had prediabetes, but not all prediabetes develops into type 2 diabetes. Of course, it’s not enough to hope you fall into the right category: without any intervention, prediabetes is extremely likely to evolve in the wrong direction. What’s happening? ...
Read MorePutting your best foot forward!
In the long run, the hyperglycemia that characterizes diabetes ends up affecting the nerves (in what is known as neuropathy) and the blood vessels, especially the capillaries. This results in a loss of sensitivity and a decrease in the natural hydration of the feet, which leads to dry skin, cracks and calluses. This means that not only are you more likely to injure your feet and not realize it right away, but you heal more slowly, and your wounds are more likely to become infected. How do you prevent problems? ...
Read MoreUnderstanding Gestational Diabetes
What is it? Gestational diabetes (or “pregnancy diabetes”) affects between 3% and 20% of pregnant women. It generally occurs in the second or third trimester of the pregnancy and goes away on its own after childbirth. Any pregnant woman can develop it, but there are a number of risk factors such as age, ethnicity, excess weight, corticosteroid use, family history and some pre-existing conditions. What’s happening? Gestational diabetes...
Read MoreHyperglycemia
When there isn’t enough insulin in your body, or when the hormone becomes ineffective, your cells are unable to use the available glucose, which then builds up in the blood. Hyperglycemia occurs when glucose levels rise above target values, i.e.: Over 7 mmol/L fasting or before a meal Over 10 mmol/L two hours after a meal Chronic hyperglycemia is what causes the long-term complications of diabetes such as blood vessel and nerve damage, blindness and kidney failure. Signs Fatigue or drowsiness ...
Read MoreProtecting Your Smile When You Have Diabetes
Diabetes increases the risk of mouth problems, but this has (almost) nothing to do with your sugar intake. The main culprit is actually hyperglycemia. The effect of blood glucose Your body can react in many different ways to improperly managed blood glucose. You produce less saliva, and the smaller amount you do produce contains more glucose, which can lead to dry mouth, ulcers, tooth decay or yeast infections. Due to hyperglycemia, there is increased glucose in the saliva which promotes the spread of bacteria, decreases nutrient...
Read MoreA Quick Overview Of Oral Medications
For type 1 diabetes With type 1 diabetes, you need to take insulin your whole life, since your body won’t produce any. It must be administered through injections or using a pump. If you’re wondering why no one has invented an insulin pill yet, that’s because stomach enzymes would make short work of it. In addition to insulin therapy, managing type 1 diabetes also requires exercising, eating a proper diet and monitoring blood glucose. Some oral medicines are sometimes prescribed to complement this. These include the following: Blood pressure medications...
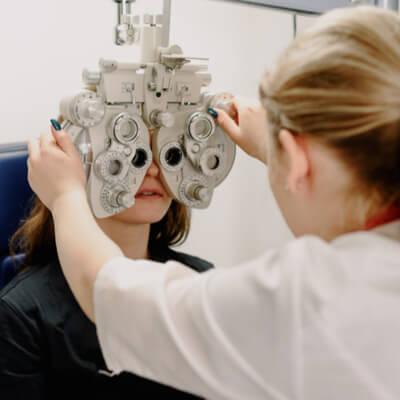
Read MoreWhen Diabetes Goes For The Eyes
It’s not a myth: diabetes can really affect eye health. Blood glucose, cholesterol levels and blood pressure are all variables that can cause serious long-term damage and, in the worst-case scenario, blindness. That’s why it’s so important to discuss this issue and focus on prevention. Here’s a quick overview to help you see the big picture. Glaucoma Glaucoma occurs when pressure builds up in the eye and damages the optic nerve and blood vessels. This disease causes a gradual loss of vision, starting with the periphery, and can...
Read MorePages
Understanding type 1 diabetes
What is it? Known as “insulin-dependent diabetes” or “juvenile diabetes", type 1 diabetes affects 5% to 10% of people living with diabetes. Type 1 diabetes requires immediate insulin treatment and occurs mostly in children and teenagers. What many people don’t know is that it can develop at any age and that it unfortunately cannot be prevented. Even today, the exact causes of the disease remain unknown. Genetics can play a role, and some environmental factors, such as viruses, can trigger the...
Read MoreUnderstanding Prediabetes
What is it? Prediabetes is when a person’s blood sugar level (blood glucose) is higher than average, but not enough to diagnose them with diabetes. Almost all people living with type 2 diabetes have had prediabetes, but not all prediabetes develops into type 2 diabetes. Of course, it’s not enough to hope you fall into the right category: without any intervention, prediabetes is extremely likely to evolve in the wrong direction. What’s happening? ...
Read MorePutting your best foot forward!
In the long run, the hyperglycemia that characterizes diabetes ends up affecting the nerves (in what is known as neuropathy) and the blood vessels, especially the capillaries. This results in a loss of sensitivity and a decrease in the natural hydration of the feet, which leads to dry skin, cracks and calluses. This means that not only are you more likely to injure your feet and not realize it right away, but you heal more slowly, and your wounds are more likely to become infected. How do you prevent problems? ...
Read MoreUnderstanding Gestational Diabetes
What is it? Gestational diabetes (or “pregnancy diabetes”) affects between 3% and 20% of pregnant women. It generally occurs in the second or third trimester of the pregnancy and goes away on its own after childbirth. Any pregnant woman can develop it, but there are a number of risk factors such as age, ethnicity, excess weight, corticosteroid use, family history and some pre-existing conditions. What’s happening? Gestational diabetes...
Read MoreHyperglycemia
When there isn’t enough insulin in your body, or when the hormone becomes ineffective, your cells are unable to use the available glucose, which then builds up in the blood. Hyperglycemia occurs when glucose levels rise above target values, i.e.: Over 7 mmol/L fasting or before a meal Over 10 mmol/L two hours after a meal Chronic hyperglycemia is what causes the long-term complications of diabetes such as blood vessel and nerve damage, blindness and kidney failure. Signs Fatigue or drowsiness ...
Read MoreProtecting Your Smile When You Have Diabetes
Diabetes increases the risk of mouth problems, but this has (almost) nothing to do with your sugar intake. The main culprit is actually hyperglycemia. The effect of blood glucose Your body can react in many different ways to improperly managed blood glucose. You produce less saliva, and the smaller amount you do produce contains more glucose, which can lead to dry mouth, ulcers, tooth decay or yeast infections. Due to hyperglycemia, there is increased glucose in the saliva which promotes the spread of bacteria, decreases nutrient...
Read MoreA Quick Overview Of Oral Medications
For type 1 diabetes With type 1 diabetes, you need to take insulin your whole life, since your body won’t produce any. It must be administered through injections or using a pump. If you’re wondering why no one has invented an insulin pill yet, that’s because stomach enzymes would make short work of it. In addition to insulin therapy, managing type 1 diabetes also requires exercising, eating a proper diet and monitoring blood glucose. Some oral medicines are sometimes prescribed to complement this. These include the following: Blood pressure medications...
Read MoreWhen Diabetes Goes For The Eyes
It’s not a myth: diabetes can really affect eye health. Blood glucose, cholesterol levels and blood pressure are all variables that can cause serious long-term damage and, in the worst-case scenario, blindness. That’s why it’s so important to discuss this issue and focus on prevention. Here’s a quick overview to help you see the big picture. Glaucoma Glaucoma occurs when pressure builds up in the eye and damages the optic nerve and blood vessels. This disease causes a gradual loss of vision, starting with the periphery, and can...
Read More