Aim for better, not perfect
Guest article by Riva Greenberg. Let's dispel a diabetes myth right now—the idea that you can manage your diabetes and blood sugar perfectly. You can't. There are so many tasks involved in managing diabetes and blood sugar that you will not be able to do them all, every day, with absolute success. For example, you won't eat perfectly all the time. There will be times an event will prevent you from being active. You may forget to take your medicine or log your blood sugar every now and then. Further, while we know keeping our blood sugar in the recommended target range helps delay or prevent diabetes...
Read MoreHow to make sense of blood sugar levels
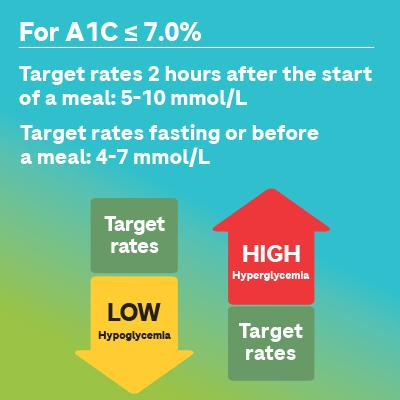
I don’t understand what my blood sugar levels mean! If you live with type 1 diabetes or type 2 diabetes, you have probably been asked to check your blood sugar a lot. But what are you supposed to be checking? How do you interpret the values you see? Managing your diabetes is easier when you know what the values mean and what you are trying to accomplish. What is the normal blood sugar level? Your doctor is the best person to ask what your blood sugar level range should be. Since everyone is different and unique, your goals may be different from the standard...
Read MoreNeuropathy: A Painful Reality
Neuropathy is one of the complications of diabetes: over time, hyperglycemia ends up damaging nerves—particularly those in the lower extremities. This can then compromise the functioning of organs such as the digestive or renal system, the heart or the genitals. Recognizing the problem and diagnosing it in time The risk factors of neuropathy share much with those of diabetes: High blood glucose High triglyceride levels in the blood Excess weight Smoking Hypertension Your health care...
Read MoreHow and Why to Get a Good Night’s Sleep
When you are getting enough sleep, you may find that you have an easier time controlling your blood sugar. You’ll be more alert during the day, have more energy, less stress, and an overall better mindset for monitoring and managing your diabetes. Consider what happens when you don’t get enough sleep. In addition to other things that may interfere with your sleep like schedule changes or stress, people living with diabetes can have potential complications with sleep. Both high and low blood sugar levels can interrupt your sleep. People living with type 2 diabetes who don’t get a good night’s...
Read MoreHow to Talk to Your Doctor
Whether you’ve been living with diabetes for years or you’re newly diagnosed, communicating with your health care team is one of the best things you can do. If you’re nervous about opening up to your doctor or pharmacist, there are some good reasons to conquer these fears. Less communication leads to measurable increases in your stress, anxiety, and possible depression. It also leads, inevitably, to less frequent and less successful diabetes management.1 Since communicating with your health care providers is proven to be good for your health, here are some guidelines for starting the conversation and keeping...
Read MorePreparing for pregnancy—good reasons to start today
Let's think into the future. Imagine sitting in a rocking chair playing with ten brand-new, tiny toes. That's the image you can remember every time you check your blood glucose, visit your doctor or say no to a glass of wine. And it's absolutely worth it. Not ready for parenthood yet? Here's what you can do now. There are several things you can do to prepare for pregnancy well before you're ready to conceive. Read about it—just not too much. When you understand the risks, you can take steps to reduce them, but it could be overwhelming if you dwell...
Read MoreUnderstanding Type 2 Diabetes
What is it? Type 2 diabetes is by far the most common: it’s the one affecting up to 90% of people living with diabetes. It is mostly found in adults (hence its nickname, “adult diabetes”), particularly in those 40 years and older. However, with the obesity epidemic currently raging around the world, it has been occurring in younger people. This type of diabetes is associated with a sedentary lifestyle, obesity and excess weight, especially in cases where there is fat accumulation in the abdomen area, but uncontrollable factors...
Read MoreTaking Good Care Of Your Skin
Living with diabetes means being more susceptible to dry skin. One reason is that high blood glucose causes more frequent urination which leads to dehydration. Given that hyperglycemia affects nerves and capillaries, you may also observe a decrease in sweating. The problem is that dry skin gets injured or cracked more easily, making it more vulnerable to infections that can create serious complications. Besides, if you’re falling prey to neuropathy, you may not notice the problem early enough. Various complications ...
Read MoreDiabetes And Depression: Warding Off The Sword Of Damocles
Being diagnosed with diabetes means it’s suddenly time to make lifestyle changes, which can feel like a loss. It’s normal to feel destabilized and experience negative feelings at first. But even beyond that initial shock, people living with diabetes are more likely to slip into depression. Greater risk Nearly 10% of people living with diabetes will experience major depression; around 30% will experience symptoms. That prevalence of depression is twice that found in populations without a chronic disease. ...
Read MorePages
How to make sense of blood sugar levels
I don’t understand what my blood sugar levels mean! If you live with type 1 diabetes or type 2 diabetes, you have probably been asked to check your blood sugar a lot. But what are you supposed to be checking? How do you interpret the values you see? Managing your diabetes is easier when you know what the values mean and what you are trying to accomplish. What is the normal blood sugar level? Your doctor is the best person to ask what your blood sugar level range should be. Since everyone is different and unique, your goals may be different from the standard...
Read MoreNeuropathy: A Painful Reality
Neuropathy is one of the complications of diabetes: over time, hyperglycemia ends up damaging nerves—particularly those in the lower extremities. This can then compromise the functioning of organs such as the digestive or renal system, the heart or the genitals. Recognizing the problem and diagnosing it in time The risk factors of neuropathy share much with those of diabetes: High blood glucose High triglyceride levels in the blood Excess weight Smoking Hypertension Your health care...
Read MoreHow and Why to Get a Good Night’s Sleep
When you are getting enough sleep, you may find that you have an easier time controlling your blood sugar. You’ll be more alert during the day, have more energy, less stress, and an overall better mindset for monitoring and managing your diabetes. Consider what happens when you don’t get enough sleep. In addition to other things that may interfere with your sleep like schedule changes or stress, people living with diabetes can have potential complications with sleep. Both high and low blood sugar levels can interrupt your sleep. People living with type 2 diabetes who don’t get a good night’s...
Read MoreHow to Talk to Your Doctor
Whether you’ve been living with diabetes for years or you’re newly diagnosed, communicating with your health care team is one of the best things you can do. If you’re nervous about opening up to your doctor or pharmacist, there are some good reasons to conquer these fears. Less communication leads to measurable increases in your stress, anxiety, and possible depression. It also leads, inevitably, to less frequent and less successful diabetes management.1 Since communicating with your health care providers is proven to be good for your health, here are some guidelines for starting the conversation and keeping...
Read MorePreparing for pregnancy—good reasons to start today
Let's think into the future. Imagine sitting in a rocking chair playing with ten brand-new, tiny toes. That's the image you can remember every time you check your blood glucose, visit your doctor or say no to a glass of wine. And it's absolutely worth it. Not ready for parenthood yet? Here's what you can do now. There are several things you can do to prepare for pregnancy well before you're ready to conceive. Read about it—just not too much. When you understand the risks, you can take steps to reduce them, but it could be overwhelming if you dwell...
Read MoreUnderstanding Type 2 Diabetes
What is it? Type 2 diabetes is by far the most common: it’s the one affecting up to 90% of people living with diabetes. It is mostly found in adults (hence its nickname, “adult diabetes”), particularly in those 40 years and older. However, with the obesity epidemic currently raging around the world, it has been occurring in younger people. This type of diabetes is associated with a sedentary lifestyle, obesity and excess weight, especially in cases where there is fat accumulation in the abdomen area, but uncontrollable factors...
Read MoreTaking Good Care Of Your Skin
Living with diabetes means being more susceptible to dry skin. One reason is that high blood glucose causes more frequent urination which leads to dehydration. Given that hyperglycemia affects nerves and capillaries, you may also observe a decrease in sweating. The problem is that dry skin gets injured or cracked more easily, making it more vulnerable to infections that can create serious complications. Besides, if you’re falling prey to neuropathy, you may not notice the problem early enough. Various complications ...
Read MoreDiabetes And Depression: Warding Off The Sword Of Damocles
Being diagnosed with diabetes means it’s suddenly time to make lifestyle changes, which can feel like a loss. It’s normal to feel destabilized and experience negative feelings at first. But even beyond that initial shock, people living with diabetes are more likely to slip into depression. Greater risk Nearly 10% of people living with diabetes will experience major depression; around 30% will experience symptoms. That prevalence of depression is twice that found in populations without a chronic disease. ...
Read More